by Tony Pearce RN.
Specialist Trichologist, National Trichology Services
As a Trichologist* specialising in female hair loss, I have treated thousands of women across the world for thinning scalp hair.
The trends I’ve observed in many women has led me to believe – despite prevailing medical opinion – there are two forms of so-called “genetic” thinning in women (female androgenetic alopecia). One is manageable but not presently curable, whilst the other may potentially be abolished.
It’s long been known that female patterned hair loss is a similar but clinically separate condition from that of male genetic balding. The hormonal conversion up to the most potent male hormone dihydrotestosterone (DHT), which has a miniaturising affect on the hair follicles across the top of the scalp, is different in males and females. So too the progression of the problem; androgen-sensitive (male hormones are termed androgens) hair follicles in women are randomly affected, thus thinning of the scalp hair occurs rather than complete baldness. Unlike males, afflicted women generally retain their frontal hairline margin as well.
True genetically inherited female androgenetic alopecia is an autosomal recessive hereditary trait affecting numbers of women within an extended family. The woman will recount a family history of her mother, grandmother/s, sisters, aunts or female cousins with a comparable thinning hair problem. These women tend to exhibit the condition after puberty or in their early twenties, particularly following childbirth. Other than low iron levels or poor dietary habits, they tend not to have any associated issues to their androgenetic alopecia.
The majority of women presenting with patterned hair thinning show (in my opinion), an acquired patterned alopecia due to the cascading affects of disordered hormonal pathways, frequently originating from problems such as oestrogen dominance, insulin resistance, or ‘leaky gut’ syndrome.
These women are 35 years + (but can be younger); mostly around or early post-menopausal and relating a common history of menstrual difficulties, pre-menstrual mood disorders, weight gain, diminished libido, sleep disturbance or headaches. Their salivary hormone profiles (SHP) will be in imbalance – usually ‘oestrogen dominant relative to progesterone – even when the oestradiol level itself is low.
In the very complex way the body’s hormones influence each other, oestrogen dominance in women results in sub-optimal thyroid function. The adrenal glands respond to this by increasing testosterone output, with ensuing loss of scalp hair in an androgenetic pattern.
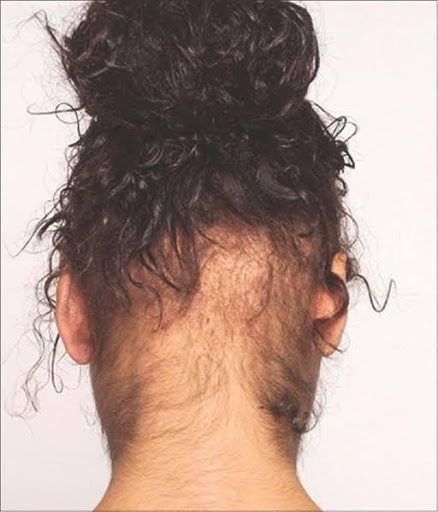
Amplified facial/body hair (hirsuitism) often accompanies patterned alopecia because follicles across the top of the scalp are androgen sensitive – causing follicle miniaturisation and hair shaft thinning (vellus hairs), whilst facial/body hair is male hormone (androgen) dependant – leading to increased growth.
Finally, stress as a cause for hair loss is often prematurely diagnosed by some practitioners, who are either unsure of what to look for or what to ask. Nevertheless severe or protracted stress from emotional, physical, chemical, or dietary causes can wreak havoc on many of the body’s vital hormones.
Adrenal gland production of cortisol is raised in times of acute stress. When this is prolonged, excess cortisol affects production of the hormones themselves and their target tissue sensitivity. Hormones that regulate ovarian/testicular function (gonadatrophins) in the respective sexes are decreased, resulting in lowered oestrogen and testosterone levels.
The pituitary gland’s production of growth and thyroid stimulating hormones are blocked by the indirect influences of excess cortisol, diminishing and disordering the conversion of the thyroid hormones from inactive to active.
Successfully treating women for hair loss problems requires careful review of their medical, nutritional, hormonal and lifestyle history undertaken in an organised and sequential way. Some specific baseline blood and SHP pathology (where appropriate) should be undertaken before deciding on a treatment regime. This will provide a clearer representation of what other areas are influencing the primary problem, and treating the cause of the condition rather than just the symptoms can then be undertaken.
*References for this article available on request.
*A qualified Trichologist has studied and successfully completed a recognised Trichology Educational Program.
About the Author: Tony Pearce is a Specialist Trichologist and Registered Nurse. He is a founding member of the Society for Progressive Trichology and the official lecturer for Analytical Reference Laboratory (ARL) for hair loss and hormone imbalance. In Australia he can be contacted on +61 2 9542 2700, or through his website at www.hairlossclinic.com.au. Copyright Anthony Pearce
Copyright Anthony Pearce 2005. *References for this article available on request